The Woolcock Institute of Medical Research
Setting patients up for CPAP success
“There’s no good reason to live with Obstructive Sleep Apnea (OSA) and lots of good reasons not to,” says Annette Truong who works in the Woolcock Therapy Centre, the Woolcock’s CPAP Clinic.
“If you don’t have a good sleep, how can you function at your best? OSA increases your risk of heart attack at an early age because your heart is not at rest throughout the night and reduced oxygen levels affect cognitive function, memory and dementia risk.”
While there are a number of treatment options for OSA, Continuous Positive Airway Pressure (CPAP) remains the gold standard when used as prescribed. The problem is, more than 50 percent of people fail with their CPAP therapy.
Annette has worked as a CPAP therapist for 15 years, guiding thousands of people through their treatment and is proud of her high success rate. With persistence and the right support, she says, most people can achieve success.
TAKING THE FIRST STEP
The right support means working with people who have the clinical skills and experience to guide you in the early stages of treatment.
“At the Woolcock Therapy Centre, we have experienced therapists who have a lot of knowledge about the sleep science behind CPAP, not just knowing how to turn on and turn off the machine or putting a mask on. If it doesn’t work straight off, patients get frustrated. They’re already suffering from lack of sleep and sometimes reluctant about CPAP. If they’re alone, if there’s no-one there to help them in those first weeks, then they won’t settle well.”
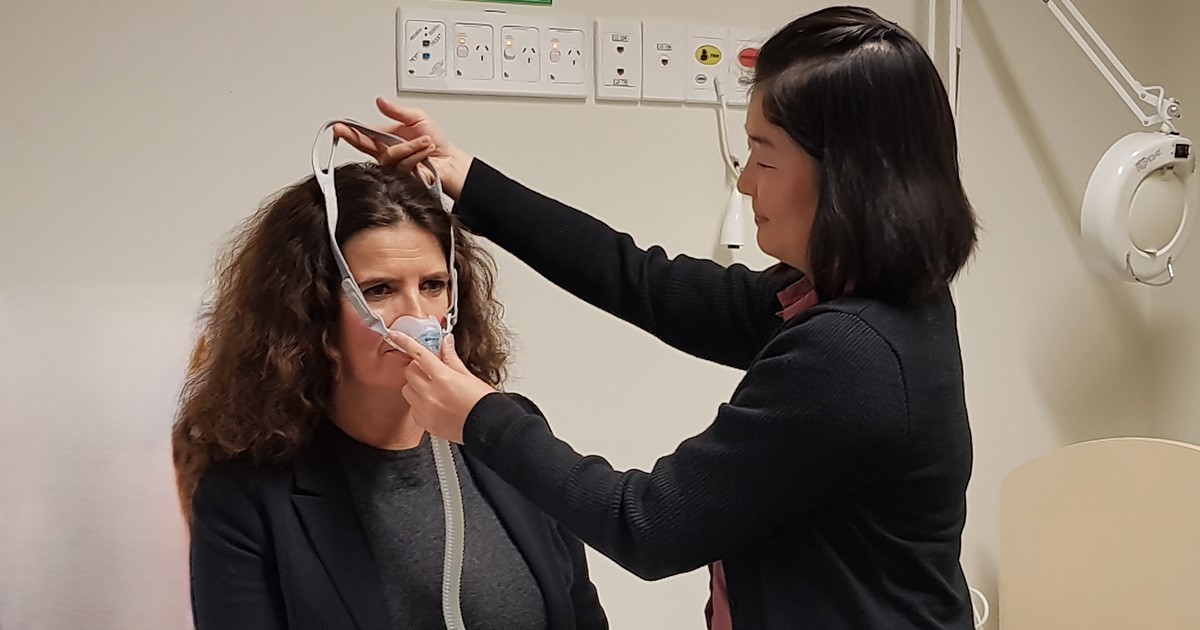
The first step is picking the right mask for the patient from the 20-30 that are currently available. That means working with someone who has the experience to ask the right questions, take into account the different sizes of mask, the shape and size of your face, how many wrinkles you have, how much facial hair, all of which play a part in determining what will be the best fit.
To those who don’t think they could ever sleep well with a mask Annette says: “You never know until you try. I’ve had a lot of patients who’ve come in with a negative mindset and have been successful with CPAP. What often gets people through that first barrier is knowing that it’s just that 1-2 minutes it takes to fall asleep that they’ll be aware of the mask on their face. That’s how quickly someone with severe OSA falls asleep because they’re so exhausted. And, after you fall asleep with CPAP, you stay asleep. For that six or eight hours, you wouldn't even know that there’s a mask on your face because you’re getting the good sleep that wasn’t possible with your OSA without CPAP.”
In the past 10 years there have also been big improvements in mask technology. Any mask will have to cover your nose and mouth, so they won’t be getting any smaller, according to Annette, but the way they mould to your face and the materials used now mean they feels like skin-to-skin – nice and soft.
Want to stay up to date with our research on sleep and respiratory conditions?
Sign up to our monthly newsletter
REACHING THE GOAL
Beyond the correct mask and machine, Annette says setting realistic goals and working together with your CPAP therapist is key to success.
“In our first appointment, we spend an hour covering every possible detail from masks, to air pressure, comfort settings and compliance so patients know what to expect. A lot of that is about expectations. If they can't sleep at first, it's OK. Everyone is different. Even after a week or two, you can use CPAP and you can use it well but you may not feel the benefit. That's why we have a four-week trial period. With time and persistence, patients will settle and it will work.”
All patients return after two weeks for a follow-up and again at the end of the four-week trial. In between, if a patient is having problems they are encouraged to ring the Centre and Annette and her colleagues can access the sleep data on their CPAP machine remotely, review it and provide recommendations on how it might work better.
“When it comes down to it, you can have a good machine but if you don't know how to use it, it's useless. You can turn it on, but if you haven't got the right mask, the right pressure, the right comfort settings, then you’re not going to sleep better. These days the machines come with up to 10 different settings and it’s getting those right that makes it work. That’s why it’s so important to have the advice and support that we provide.”